Project Update: Inclusive Health Communication on Infectious Disease in Disability Group Homes

Image: DC Studio on Freepik
Since late 2020, our team has been conducting a large research project into the way that information about infectious disease is communicated in disability group home settings. We have interviewed disability group home residents and support workers, and collaborated with service managers and therapists. We have reviewed any previous research about the involvement of people with intellectual disability in the prevention and management of infectious disease. We have also reviewed the local, Australian, and international policies that were developed in response to COVID-19, to see how relevant they were for disability accommodation services.
In this post, I want to share with you the findings from our interview studies. A lot of what we have learned matches what has been reported in related international research. One key theme concerns the profound impact of the pandemic on the lives of group home residents and staff. Reported impacts on residents have included a loss of control, routine and quality of life, reduced social, economic and community participation, a decline in mental and physical health, and reduced access to health and other disability services. Negative impacts on residents’ interpersonal relationships with friends, family, other residents, and staff were also reported. Residents had been frustrated by lockdowns and wanted more information about the public health restrictions in place, particularly when they would be lifted or changed. Similar concerns have been observed and reported internationally since the start of the pandemic.
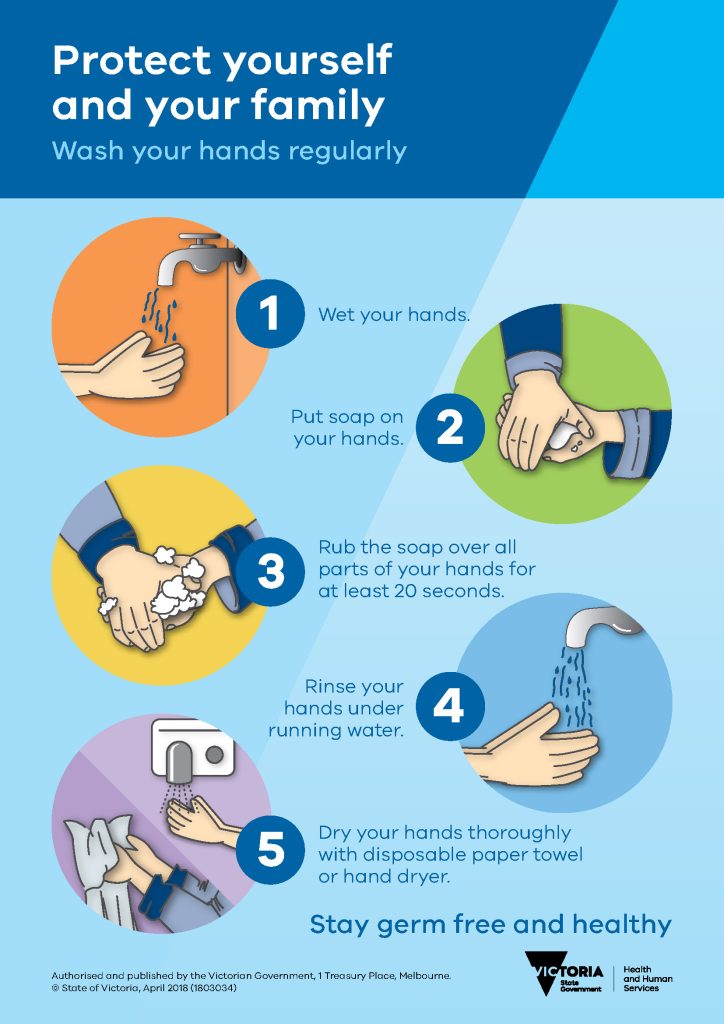
Image: DHHS Victoria.
Our project has generated some novel preliminary insights into the way that public health information is communicated in group home settings. Existing research and clinical reports about public health interventions for people with intellectual disability have primarily focused on a one-way flow of information from experts (e.g., Governments, health professionals and service providers) to people with intellectual disability. Training programs and accessible information materials are two common examples of this model. However, our research suggests that SDA staff and residents do not rely solely on these lines of communication to make informed decisions about their health behaviour. Instead, we have learned that understandings about COVID-19 are formed through complex, multi-way dialogue between residents, staff, and people outside the home. During these interactions staff and residents share their own perspectives and knowledge about COVID-19; these are sometimes expressed using words (e.g., sign language or speech) and sometimes non-verbally (e.g., through behaviours, body language, and creative or artistic expression).
Residents and staff in SDA facilities have experienced these interactions and decision-making processes while immersed in an “information soup” of televised news and press conferences, internet media, the visual and environmental artefacts of infection prevention, and the opinions of friends, family, and the broader community. The messages shared within these complex interactions and environments has been fluctuating and contradictory. Additionally, residents and their staff had varying degrees of interest in learning about COVID-19, and varying levels of control over the format and content of the information they received.
Residents and staff have shared some practical suggestions for making health information more accessible and inclusive, such as the use of videos, pictures, Auslan and alternative communication modes to support written documentation and media reporting. We have also learned about some broader factors that appear to be important for inclusive and effective health communication in SDA settings. These include:
- the diverse communication support needs and preferences of staff and residents,
- the role that trust and familiarity between communicators plays in sharing and forming understandings about health,
- the way that fundamental human rights such as safety, health, autonomy, and personal belief are acknowledged and addressed in public health interventions and messaging,
- the way that residents and staff view their own ‘duty of care’ in protecting members of their community within and beyond the group home.
- the degree to which people with intellectual disability or complex communication needs are supported to seek information, express ideas, and take action on public health issues like COVID-19.
We are continuing to explore these themes in the later phases of our research, including a Delphi survey (to set practice priorities), and Knowledge Translation Working Parties (looking at how this information could be used in a range of healthcare and disability service settings). Our observational studies within group homes is also ongoing. If you would like to be part of any of these projects, please don’t hesitate to get in touch: [email protected]